Managing Your
Performance Horse’s
Joints
A comprehensive look at options for keeping equine athletes with arthritis on the move
By Stacey Oke, DVM, MSc
Sponsored by:
PHOTO: Getty Images
You and your horse enjoy leading an active lifestyle, routinely preparing for and participating in competitions. One extremely common consequence of that lifestyle is osteoarthritis (OA). Here are some fast facts about equine OA:
Osteoarthritis is the most common cause of lameness in horses, responsible for approximately 60% of lameness cases.
horses in the United States are estimated to be currently affected.

Equine osteoarthritis contributes to massive economic losses as well as horse attrition.

This is not an old horse disease—it commonly occurs in young, active performance horses.
“Horses can and do develop OA from an early age, and almost all performance horses will inevitably suffer from a certain degree of OA, particularly in articulations such as the distal tarsal (lower hock) joints,” says Dr. José M. García-López, associate professor of large animal surgery at the University of Pennsylvania’s New Bolton Center.
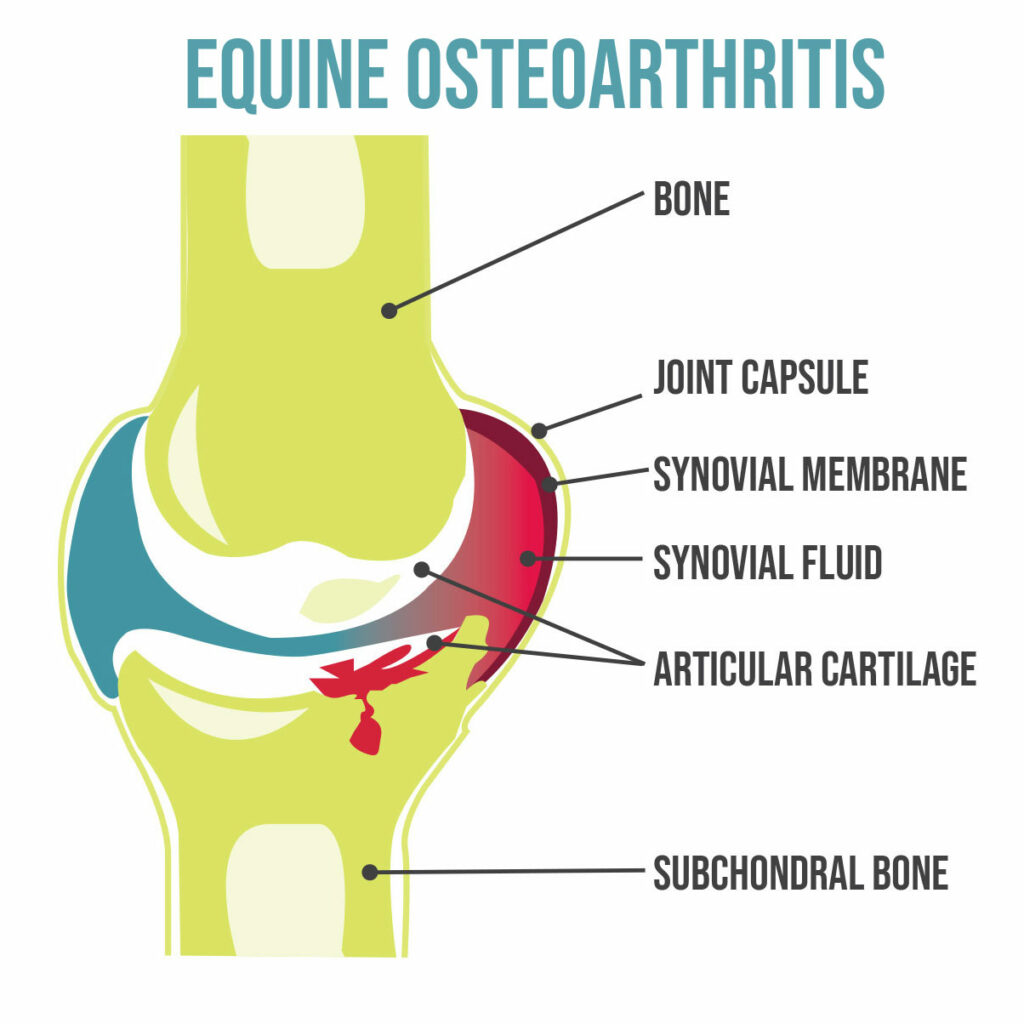
By definition, OA refers to the degeneration of articular cartilage that lines the ends of bones inside joints. That layer of articular cartilage is what cushions the bones to dissipate concussive forces as the horse moves, permitting smooth, frictionless motion.

José M. García-López, VMD, Dipl. ACVS, ACVSMR
García-López is associate professor of large animal surgery at the University of Pennsylvania’s New Bolton Center, in Kennett Square. His area of focus is equine orthopedics, including arthroscopy and fracture repair, lameness diagnosis and treatment, and advanced imaging.
While we used to focus just on the joint’s articular cartilage, we now know OA is a “whole joint” disease, also affecting the layer of bone lying directly beneath the cartilage (subchondral bone), the synovial membrane lining the joint, the joint capsule, supporting ligaments, and other structures such as the menisci in the stifle joints.
“Inflammation of the joint capsule (capsulitis) or the synovial membrane (synovitis) stemming from trauma, repeat concussion, intra-articular ‘chip fractures,’ etc. increases the production of catabolic proteins,” García-López explains. “These proteins, such as cytokines and interleukins (IL), are responsible for degrading cartilage.”
One interleukin that is of particular importance in the development of OA is IL-1 beta (IL-1β).
“IL-1β is responsible for upregulating other inflammatory mediators that target the destruction of the main components of cartilage, such as collagen and proteoglycans,” he says. “In addition, IL-1β will, at the same time, downregulate the ability of the cartilage to repair itself. IL-1β thereby creates a catabolic environment with the ultimate result being the loss of articular cartilage, which is the hallmark of OA.”
Owners and their veterinarians should, therefore, take steps to prevent joint trauma and inflammation. When OA can’t be prevented, early intervention should be implemented to control the horse’s discomfort and slow the progression of this incurable disease. In this article we’ll focus on practical strategies aimed at preventing OA in athletes and how to manage OA once the inflammatory cascade has been initiated.
PHOTO: Getty Images
Preventing Arthritis in Performance Horses
Seize the Weigh!
Believe it or not, weight management is one of the most important and relevant ways to prevent arthritis in horses. One widely used statistic in human medicine for imparting the importance of body weight on joint health is that for every pound increase in body weight, there is a fourfold increase in knee joint compressive forces (Messier et al., 2005).
“Our equine athletes can similarly suffer from the effects of increased body weight and improper conditioning that will result in an inappropriate degree of loading or stress to the cartilage during exercise,” says García-López.
Equine researchers have found as many as 70% of horses in some populations are overweight and obese, and excess condition is now widely accepted throughout the industry as “the norm” (Rendle et al., 2018).
Obesity is rampant in not only the leisure horse population but also in performance horses. Rendle relayed that 41% of 332 horses and ponies competing at a national level were overweight and an additional 21% were obese. That means a total of 62% of the competitive show and dressage horses were carrying excess body weight. In a more recently published study, 35% of 377 ponies at a national hunter competition, classified as athletic and elite ponies, were obese (Pratt Phillips et al., 2023).
Owners aren’t the only culprits accepting of overweight horses. In a recently published survey, researchers found that horse show judges also lean toward favoring an obese body condition (Munjizun and Pratt Phillips, 2022). Judges in that study were given the opportunity to evaluate 13 photographs of horses with various body condition scores. Of the five horses veterinary experts characterized as obese, the judges classified them as only overweight. For the three horses that were overweight, judges felt they were average. Finally, 91% of surveyed judges deemed one of the horses as thin when a veterinarian considered him average.
Because obesity is one of the greatest modifiable risk factors for OA, owners should familiarize themselves with the nine-point Henneke body condition scoring scale and seek advice from their veterinarians or from equine nutritionists.
Joint Supplements to Prevent Equine Arthritis
Many owners don’t consider oral joint health supplements for horses until after clinical signs of OA develop. Evidence in other species, however, suggests certain supplements could potentially confer prophylactic (preventive) benefits. In a commonly cited study supporting the protective features of oral joint health supplements (Canapp et al., 1999), dogs received an oral glucosamine hydrochloride-chondroitin sulfate supplement for 21 days. At that point, the researchers induced synovitis by injecting a caustic chemical into the dogs’ radiocarpal (wrist) joints. The research team found that prior treatment with glucosamine and chondroitin sulfate had a protective effect against chemically induced synovitis and associated bone remodeling and reduced lameness.
Horses, however, are not large dogs, and we cannot assume results from canine studies directly translate to equine patients.
“Evidence regarding oral supplementation in equine patients is lacking,” says García-López.
Preventive Intra-Articular Therapies
In a survey, 423 board-certified equine practitioners reported they used orthobiologic therapies as “preventive treatment” in a very small number of cases (Knott et al. 2021). The term orthobiologic refers to biological substances derived from compounds naturally found in the body to help musculoskeletal injuries heal quicker.
“We do not currently have any evidence that using intra-articular products, regenerative or otherwise, in the normal joint prevents OA,” says Dr. Kyla Ortved, assistant professor of large animal surgery at New Bolton Center. “However, it is likely that early recognition of joint inflammation followed by targeted treatment can help limit the inflammatory cascades that potentiate the development of OA.”
In one study
and an additional

Many owners don’t consider oral joint health supplements until after clinical signs of equine osteoarthritis—heat, pain, swelling, and decreased range of motion—develop.

Kyla Ortved, DVM, PhD, Dipl. ACVS, ACVSMR
Ortved is an assistant professor of large animal surgery and the Jacques Jenny Endowed Term Chair in Orthopedic Surgery at the University of Pennsylvania’s New Bolton Center, in Kennett Square. Her research focuses on establishing regenerative therapies to improve musculoskeletal healing using the horse as a model for human disease.
PHOTO: Flickr CC/Cody Klein
Managing Arthritis in Performance Horses
Identifying equine arthritis early allows owners and their veterinarians to take steps to slow its progression and maximize the longevity of the horse’s athletic career. Ideally, researchers would identify disease-modifying OA drugs (DMOADs) that could stop or reverse damage to the articular cartilage, allowing it to heal. Currently, however, even orthobiologics do not meet the criteria for DMOAD, because they do not effectively reverse OA (Oo et al., 2021).
Therefore, we only have symptom-modifying OA drugs, or SMOADs, which improve the clinical signs of OA, such as heat, pain, swelling, and decreased range of motion. In other words, despite having an arsenal of therapies at our disposal, OA remains incurable, and we can only slow its inevitable progression.
Veterinarians currently recommend a multimodal treatment approach for horses diagnosed with OA. The veterinarian and owner/trainer must work together to select the management tactics they ultimately use. We’ll describe some of the available evidence-based options in the following sections.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)

These ubiquitous drugs, such as phenylbutazone (Bute), keep inflamed joints comfortable and are widely used as part of the approved multimodal treatment approach to OA. In older pasture pets NSAIDs can certainly help control comfort and maintain quality of life. In performance horses, however, experts agree that NSAIDs should not form the base of the treatment pyramid.
“I think that NSAIDs can have a place in performance horse management,” says García-López. “These can safely be used at a low dose and while monitoring the overall health of the horse, either during conditioning or rehabilitation from an injury.”
Intra-Articular Therapies
In lieu of relying on NSAIDs to help maintain joint health, veterinarians often use intermittent intra-articular therapies to control joint discomfort in performance horses. In a recently published survey 407 equine veterinarians provided information regarding some of the more popular therapies currently being used in performance horses (Zanotto and Frisbie, 2020). Based on that survey, corticosteroids—primarily triamcinolone and methylprednisolone—are still one of the first-line intra-articular therapies. Practitioners frequently co-administer hyaluronic acid with those intra-articular corticosteroids.

"If I have a horse that has lameness or pain attributable to a particular joint, I won't hesitate to use orthobiologics in the early stages of disease."
Dr. Kyla Ortved
Despite these tried-and-true articular therapies, Ortved says the tides are changing.
“I think using orthobiologics early in the disease process is better because they are designed to prevent further damage and promote healing,” she says. “If I have a horse that has lameness or pain attributable to a particular joint, I won’t hesitate to use orthobiologics in the early stages of disease. And I feel more comfortable using these before jumping to steroids as I think they are more protective of the cartilage.”
For OA, orthobiologics (biologics, biological therapies), include the following:
Autologous conditioned serum (ACS, interleukin-1 receptor antagonist protein, or IRAP)
The veterinarian collects a small volume of blood from the patient and mixes it with special beads included in a commercial ACS kit. The incubation process stimulates the production of anti-inflammatory molecules, most importantly IRAP. The veterinarian then injects this “conditioned” serum into the target joint to inhibit inflammation caused by IL-1β.
Platelet-rich plasma (PRP)
The veterinarian collects a sample of the patient’s blood and centrifuges it to separate and concentrate the horse’s platelets. Those platelets contain a large variety of growth factors that have anti-inflammatory and other properties.
Autologous protein solution (APS)
This technique combines the benefits of ACS and PRP. The veterinarian uses a two-step centrifugation process on an equine patient’s blood sample to concentrate both platelets and IRAP into a single injectable product.
Stem Cells
After collecting stem cells from bone marrow or adipose tissue, the veterinarian processes and injects these cells directly into joints where they exert anti-inflammatory and immune-modulating properties and recruit other stem cells within the joint to facilitate healing.
Eighty-seven percent of the 407 equine veterinarians Zanotto and Frisbie surveyed reported having patients that benefited from intra-articular biological therapies. And 45.7% of veterinarians indicated their primary reason for choosing a intra-articular biological therapy over a corticosteroid was long-term efficacy. Autologous conditioned serum, PRP, APS, and stem cells were used by 83.38%, 72.5%, 53.8%, and 53.7% of equine practitioners, respectively.
PHOTO: Getty Images
Rounding Out the Treatment Plan
With daily NSAIDs off the table for horses with arthritis actively involved in competition, what else can we reach for to keep performance horses on the road to success?
Other Intra-Articular Therapies
Another intra-articular product available for horses is Polyglycan, which is essentially a synovial fluid replacement product. “I use Polyglycan, which is made of a patented formulation of hyaluronic acid, chondroitin sulfate, and N-acetyl-D-glucosamine, at the end of any elective arthroscopic procedure and also as my hyaluronic acid fluid replacement product of choice,” says García-López, citing a 2009 study out of Colorado State University that showed Polyglycan to have the potential to have both symptom- and disease-modifying effects.
Polyacrylamide hydrogels are also available for horses with OA and gaining popularity. Polyacrylamide gels are synthetic products, not orthobiologics, injected into the joint to provide lubrication and shock-absorbing properties. In one study of a 2.5% polyacrylamide hydrogel product, researchers reported that 83% of treated horses were lame-free at four, six, and 12 weeks following administration.
Despite study findings, García-López believes more unbiased research is needed on these products.
“There is subjective evidence that these gels can create fibrosis of the synovium and granulation tissue formation that, in turn, can affect the composition of the synovial fluid, which is the main source of nutrition to the cartilage in adult articulations,” says García-López. “This family of gels could be considered in end-stage cases of OA but maybe not in early or moderate cases of OA.”
Intramuscular Therapies
Our sources remind us not to forget that OA management is multimodal, and intramuscular (IM) polysulfated glycosaminoglycan (Adequan) is still recommended by veterinarians.
“I like to use Adequan in performance horses,” says Ortved. “I generally recommend 500 milligrams IM every four days for seven treatments every six months or at time of injury.”
García-López agrees with Ortved, adding, “In horses that have either early signs of joint inflammation or OA without significant morphologic changes, I like to place them on a course of IM Adequan for the one dose every four days for seven treatments. This has shown good objective evidence for helping restore the ‘steady state’ between production and destruction of cartilage components. Basically, it is quite helpful to keep what is good, good.”
Physical and Alternative Therapies
Again, not to be outshone by fancy, flashy biologics, many other therapies help round out a performance horse’s joint therapy plan.
“I think physical therapy is a huge part of management and something we need more data on and help from specialists integrating into practice,” Ortved says.
"If I have a horse that has lameness or pain attributable to a particular joint, I won't hesitate to use orthobiologics in the early stages of disease."
Dr. Kyla Ortved
Examples of such physical therapies include postural exercises and exercises designed to improve coordination and proprioception, target muscle atrophy/weak muscles (potentially secondary to joint discomfort and disuse), and increase joint stability through conditioning. Additional therapies you might consider to help keep performance horses’ joints comfortable include extracorporeal shock wave therapy (ESWT), laser, and acupuncture/electroacupuncture.

Physical therapies and conditioning, such as hillwork, can help round out a performance horse’s joint health plan.
Oral Joint Health Supplements
Horse owners often offer joint supplements, making these products one of the most popular types of supplement on the market. Of the studies performed in horses, evidence does support the use of some ingredients, such as (but not limited to), glucosamine hydrochloride, chondroitin sulfate, and avocado-soybean unsaponifiables (ASU). The science and regulatory oversight of many products, especially supplement quality and testing, however, do not match the industry’s enthusiasm for them. In other words, a lot of joint supplements do not contain the type or amount of ingredient listed on the label, and many products have not been tested in clinical trials to demonstrate efficacy.
“Nutraceuticals should not replace treatment with other products such as Adequan, Legend, Polyglycan, or intra-articular therapy, whether it is with an orthobiologic or corticosteroid.”
Dr. Jose Garcia-Lopez
In light of quality and efficacy concerns, some veterinarians recommend owners allocate their “joint health budget” more toward injections (intra-articular and intramuscular).
“The data regarding the use of oral nutraceuticals in horses is truly lacking. When I discuss these products with owners, I mention that if they don’t mind the extra expense, they can try oral nutraceuticals such as Cosequin,” says García-López. “However, nutraceuticals should not replace treatment with other products such as Adequan, Legend, Polyglycan, or intra-articular therapy, whether it is with an orthobiologic or corticosteroid.”
PHOTO: Taylor Pence Photography
Managing OA Is a Joint Effort
Regardless of which modalities an owner/veterinary team elects to use when approaching joint health, our sources recommend approaching OA as not just a cartilage or even a joint issue but, rather, a “whole-horse disease.”
“Conditioning, shoeing, nutrition, and overall health all play a role in joint health,” says Ortved.
“Conditioning cannot be overlooked,” adds García-López. “Equine athletes have their entire weight, which biomechanically increases exponentially during exercise, transferred through one or two limbs at a time. They need to be properly conditioned in order for all musculoskeletal components, including muscle, tendon, ligament, bone, and cartilage, to share the load adequately.”
No matter which strategies you and your veterinarian ultimately integrate into an athletic horse’s joint-health plan, as a team you must critically evaluate and reevaluate that plan regularly to make sure you’re optimizing each individual horse’s treatment to his particular needs, balancing equine ability with fragility.
Sponsored Message:
Winning in Their Blood, Polyglycan® in Their Joints!
Polyglycan® (Hyaluronic Acid, Chondroitin Sulfates C4 & C6, N-acetyl-D-glucosamine Sterile Solution) is a patented three-component formulation from Bimeda® designed to replace lost or damaged synovial fluid. It contains naturally occurring components of the synovia that play a central role in maintaining the homeostatic environment of the joint. The patented three-component formula has demonstrated characteristics beyond any of these components used individually. Polyglycan® is specifically formulated to have the same viscosity and lubricating properties as natural equine synovial fluid.
Polyglycan® has been administered extensively to horses competing in a variety of disciplines. This population includes professional rodeo horses, cutting horses, reining horses, working cow horses, racehorses, and horses in the English disciplines. The most trusted veterinarians in the industry have used and continue to use Polyglycan® as a standard in both postsurgical and treatment of typical inflammatory conditions of the joint. Robert W. Brusie, DVM, Dipl. ACVS, of Palm Beach Equine Clinic, in Wellington, Florida, notes that, “Additionally, we have not experienced the occasional joint flare seen in other products.” Regarding treatment efficacy, C. Wayne McIlwraith, BVSc, PhD, Dipl. ACVS, ACVSMR, and David D. Frisbie, PhD, Dipl. ACVS, ACVSMR, both with Colorado State University’s Orthopaedic Research Center, state that “… joints of Polyglycan®-treated horses had fewer microscopic articular cartilage abnormalities as well.”
“I use Polyglycan® exclusively (other than biologics) in joint therapy. In other words, Polyglycan® is my “go to” medication,” says Brusie. Robert J. Hunt, DVM, MS, Dipl., ACVS, of Hagyard Equine Medical Institute, in Lexington, Kentucky, says, “I began using Polyglycan® in a clinical setting over 10 years ago, initially as a postsurgical lavage following arthroscopic surgery. Soon afterward I began routine administration on a weekly or biweekly basis on athletes with musculoskeletal maintenance issues as well as young developing horses with developmental orthopedic issues. I have continued to use Polyglycan as a standard postoperative treatment as well for essentially all of my orthopedics.”
Over six million doses have been administered by trusted veterinarians since 2006. These trusted veterinarians use and continue to use Polyglycan® as their standard course of treatment.
Credits
Stacey Oke
 Stacey Oke, MS, DVM, is a practicing veterinarian and freelance medical writer and editor. She is interested in both large and small animals, as well as complementary and alternative medicine. Since 2005, she’s worked as a research consultant for nutritional supplement companies, assisted physicians and veterinarians in publishing research articles and textbooks, and written for a number of educational magazines and websites.
Stacey Oke, MS, DVM, is a practicing veterinarian and freelance medical writer and editor. She is interested in both large and small animals, as well as complementary and alternative medicine. Since 2005, she’s worked as a research consultant for nutritional supplement companies, assisted physicians and veterinarians in publishing research articles and textbooks, and written for a number of educational magazines and websites.
Editorial Director: Stephanie L. Church
Managing Editor: Alexandra Beckstett
Digital Editor: Haylie Kerstetter
Art Director: Claudia Summers
Web Producer: Jennifer Whittle
Publisher: Marla Bickel