Horses’ heightened flight response combined with their long, spindly legs creates a perfect storm for abrasions, contusions, punctures, and lacerations. And lack of veterinary involvement when managing wounds in horses, particularly on the lower limbs, can spin those storms into hurricanes.
Richard Birnie, BVMBVS (Hons), MRes, MRCVS, a veterinary intern at REC Equine Specialists, in Sydney, New South Wales, Australia, says multiple researchers have reported that traumatic wounds in horses are the second-most-common emergency veterinarians see, with colic being the first.
These traumatic wounds vary remarkably in their presentation, and simple visual inspection doesn’t always reveal the extent of the injury.
“Inappropriate management of a wound can delay the institution of appropriate therapies, negatively affect outcome, and dramatically increase the cost of treatment,” says Birnie, who conducted research on equine wound treatment while studying for his veterinary degree at the University of Nottingham, in the U.K. “The prognosis for return to function can also decrease, while the time taken to return to work can be extended due to the development of complications.”
How To Handle Equine Wounds Isn’t Always Clear-Cut
If you’re like many horse owners, your barn has a cupboard full of first-aid supplies, salves, ointments, sprays, and powders. Together with self-adhesive wrap, Dr. Google, and advice from your horse-owning friends, you might feel appropriately armed to deal with an array of wounds, but Birnie’s research results suggest otherwise.
While horse owners’ intentions are good, many don’t call their veterinarian right away, potentially creating more problems than they’re solving. To assess owners’ understanding of equine wounds, Birnie and his University of Nottingham colleagues, including Professor Sarah Freeman, BVetMed, PhD, Cert. VA, Cert. VR, Cert. ES, Dipl. ECVS, FHEA, MRCVS, surveyed more than 1,000 horse owners about how they would manage seven hypothetical wound scenarios (e.g., puncture wounds, kick injuries, degloving injuries).
“Owners stated that the most important factors influencing their decision to seek veterinary advice were the depth and location of the wound, as well as the amount of bleeding,” Birnie says.

However, when presented with a hypothetical wound situation, survey participants didn’t consistently put this methodology into practice. For example, owners were unskilled at recognizing the severity of deep puncture wounds over synovial structures, such as a joint or tendon sheath. According to survey results, less than 25% of surveyed horse owners thought these small punctures were a high priority, and 34% said they did not think a small puncture required any veterinary treatment.
“Despite appearing small and innocuous at skin level, if these small wounds extend deeper and involve synovial structures, it can be potentially catastrophic for the horse’s overall prognosis,” explains Birnie.
Besides the inability to recognize the severity of certain wounds, Birnie et al. found more than half the survey respondents chose to apply some form of contraindicated first-aid, relating specifically to wound cleaning, medicating, and bandaging.
Birnie’s survey results show that some owners used overly concentrated and, therefore, cytotoxic (toxic to cells) chlorhexidine solutions to clean wounds, which can impair and slow healing. They also commonly applied silver sulfadiazine to wounds; however, some silver products can also be cytotoxic and might not be appropriate for all wounds.
Overall, this work highlights the importance of veterinarian involvement in equine wound management.
Richard Birnie
BVMBVS (Hons), MRes, MRCVS

Richard Birnie is a veterinary intern at REC Equine Specialists, in Sydney, New South Wales, Australia. While a veterinary student at the University of Nottingham, in the U.K., he performed research on horse owner attitudes about equine wound management. He presented his team’s findings during the British Equine Veterinary Association’s 2020 Clinical Research Week.
Less than
Less than
What Owners Should Do for Equine Wounds
CREDIT: Peggy Marsh
Dean Hendrickson

Dr. Dean Hendrickson is professor of equine surgery at Colorado State University’s College of Veterinary Medicine and Biological Sciences, in Fort Collins. His areas of expertise center around equine wound care and minimally invasive surgery.
- Move your horse to a safe place to limit further injury and keep him quiet.
- Use clean towels to apply direct pressure if the wound is actively bleeding. Covering the wound will also avoid further contamination with dirt, feces, and debris.
- Refrain from cold hosing (this can drive foreign material further into the injured tissues). Instead, flush the wound gently to remove gross debris.
- Do not apply a tourniquet to stop bleeding unless directed by your veterinarian.
- Restrain from placing any topical product that might be contraindicated. This includes chlorhexidine, hydrogen peroxide, and iodine. In fact, if you don’t know exactly what a topical agent does, don’t use it.
“The most important thing is to clean the wound well without antiseptics to minimize further trauma and necrosis of the wound,” says Dr. Dean Hendrickson of Colorado State University. “The majority of antiseptics have been shown to actually increase infection and/or slow wound healing.”
A Prescription for Infection-Free Wound Repair
How your veterinarian manages your horse’s wound depends heavily on the structures involved and level of contamination. Most wounds require debridement, which is the removal of dead, damaged, or infected tissue and foreign material to improve the healing potential of the remaining healthy tissue. But, in all reality, you’re probably most concerned with what medications you will need to give your horse for the next week or so.
Our experts agree that the days of rote and routine antibiotic administration are long over.
“With appropriate lavage, debridement, and debridement dressings, many equine wounds do not actually require antibiotics, including topical antimicrobials placed directly on the wound,” says Dr. Lucas Pantaleon.
“Both the overuse and unnecessary use of antibiotic drugs has resulted in antimicrobial resistance” in pathogens (disease-causing organisms), adds Dr. Val Edwards-Jones, an emeritus professor of medical microbiology at Manchester Metropolitan University, in the U.K. “This misuse of antibiotics now threatens both humans and animals due to the dearth of new antibiotics on the horizon. We are returning to the pre-antibiotic era where simple infections could result in death,” because existing antibiotic drugs have been rendered less effective, even ineffective. “Antibacterial stewardship in all health care professions must therefore be embraced, and the indiscriminate use of these medications needs to stop.”
Dr. Val Edwards-Jones says scientists across a variety of health care sectors agree the best way to use antibiotics is to choose the right antibiotic for the right patient, at the right time, with the right dose, and for the right route, causing the least harm to the patient and future patients.
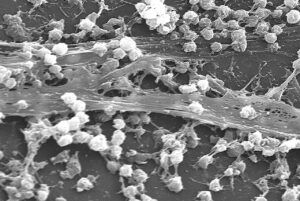
Complicating antibiotic efficacy, some bacteria found in chronic wounds also produce biofilm—a three-dimensional matrix of extracellular substances that forms a barrier that antibiotics have extreme difficulty penetrating. Biofilm delays healing, which can promote the development of chronic wounds.
“We have shown that over 80% of chronic wounds in humans have a biofilm that does not cause overt infection but prevents wound healing,” says Edwards-Jones. “Biofilm is attached to the surface of the wound and encapsulates the microorganisms. Data show that almost 1,000 times more antibiotic is required to remove bacteria from a biofilm. Effective debridement, however, is a great way to remove biofilm and bioburden.”
In addition to concerns related to antibiotic resistance, systemically administered antibiotics—those given intravenously, intramuscularly, and orally—can result in antibiotic-associated diarrhea (AAD).
“Antibiotic-associated diarrhea causes high rates of complications and has a high mortality rate,” says Pantaleon, adding, “most any class of antibiotic can cause AAD in horses.”
Pantaleon says research shows that, to date, tetracyclines, macrolides, cephalosporins, fluoroquinolones, trimethoprim-sulfonamides, aminoglycosides, chloramphenicol, and β-lactams can all cause colitis (inflammation of the colon—the portion of the large intestine connecting the cecum with the rectum—that can lead to diarrhea, proliferation of harmful bacteria, and even death in severe cases) in horses. Administering antibiotics to a horse causes different degrees of dysbiosis—an imbalance of the normal microbial population in the hindgut (the portion of the GI tract after the small intestine).
Lucas Pantaleon
DVM, MS, MBA, Dipl. ACVS

Dr. Lucas Pantaleon, of DVM One Health, in Versailles, Kentucky, is an animal health industry advisor with an expertise in infection prevention and biosecurity.
Dr. Val Edwards-Jones
PhD, CSci, FIBMS

Val Edwards-Jones is emeritus professor of medical microbiology at Manchester Metropolitan University, U.K.; a visiting professor at institutions in the U.K. and Russia.; and a clinical director, technical director, and independent microbiology consultant with various labs and test facilities. Her research interests are wound infection, toxic shock syndrome, alternative treatment strategies, essential oils as antimicrobial agents, and rapid diagnosis of infection using mass spectrometry.
Antibiotic-Free Management of Wounds
CREDIT: iStock
Veterinarians have various bandaging techniques at their disposal to abrogate the need for carte blanche antibiotic administration, as well as products such as honey and silver.
“Studies show that honey and nanosilver are very effective in bacterial reduction without any known resistance,” says Hendrickson. “If they are coupled with good cleaning (without antiseptics) and debridement, these can be very effectively used as long as your veterinarian makes sure the synovial structures are not involved.”
Manuka Honey
Andrew Dart
BVSc, PhD, Dipl. ACVS

Dr. Andrew Dart is a professor and director of the research and clinical training unit at University of Sydney, in Australia. His research has included topical wound management.
Over the past several years, using manuka honey (produced with nectar from the flowering manuka tree Leptospermum scoparium) to manage wounds has piqued the interest of veterinarians, particularly in the face of growing antimicrobial resistance.

Researchers have studied topical manuka honey, a medical-grade honey with a UMF (unique manuka factor) based on its antimicrobial activity due to the α-dicarbonyl compound methylglyoxal (MGO), extensively.
Manuka honey has an osmotic effect due to its high sugar content (it dries out bacteria), is acidic and therefore inhibits bacterial growth, and contains bactericidal enzymes. Further, Dr. Andrew Dart and colleagues from The University of Sydney, in Australia, have reported that manuka honey, unlike antibiotics, breaks down bacterial biofilms (Dart et al., 2015, 2017, 2020). Manuka honey prevents biofilm formation or, if already established, disrupts it, Dart says.
Evidence indicates manuka honey promotes wound healing in addition to exerting its antimicrobial properties.
“Recent studies investigating the effects of manuka honey on second intention healing of lower limb wounds in horses have shown that wounds treated with UMF 20 manuka honey retracted less and healed faster than untreated wounds,” says Dart.
Dart recommends using medical-grade manuka honey when dealing with heavily contaminated wounds or wounds with biofilms.
He adds that some veterinarians, rather than recommending honey-laden or honey-impregnated bandages, “simply apply honey under a dressing early in the healing process. Later, manuka honey can then be applied as a thin layer on the healing granulation bed two or three times daily without a bandage.”
This latter approach might be desirable considering that bandaging can promote the development of proud flesh—exuberant granulation tissue (EGT)—even with the use of honey.
Nanosilver Technology
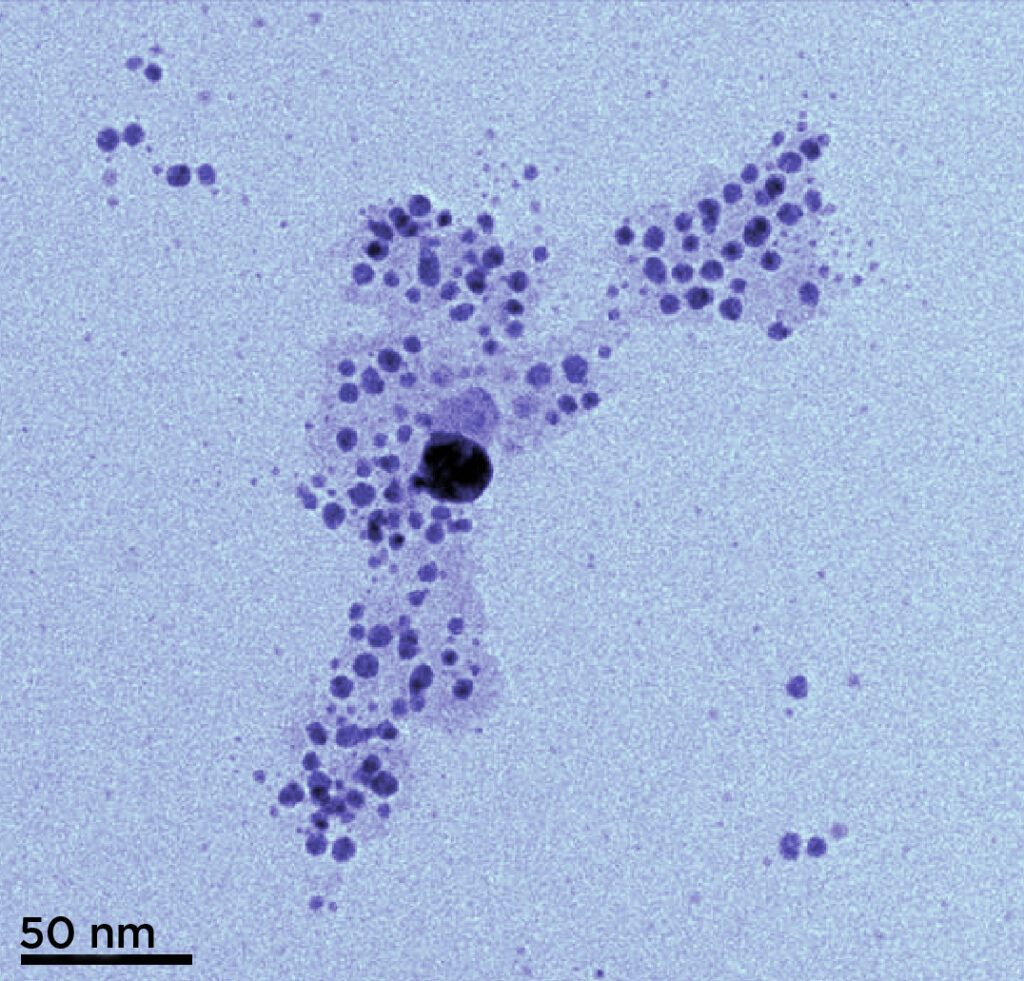
Pantaleon says practitioners often advocate for using silver products in wound management because silver ions have microbicidal effects. However, he adds, very high concentrations of silver ions—like those found in the traditional silver products that come in the form of sprays and powders—injure the cells and interfere with the healing process.
“Newer silver formulations called nanocrystalline silver have the ability to release the silver ions in a more controlled way, preventing the toxic effect on tissues,” Pantaleon explains. “Silver ions have multiple microbe-killing mechanisms. These ions, for example, can alter the membrane around bacteria, causing the bacteria to rupture and die. Also, silver ions can enter the microbes, causing deleterious effects in vital functions and also causing (pathogen) death.”
Commercial dressings impregnated with nanosilver:
- Are nontoxic to cells involved in wound healing;
- Have broad-spectrum antimicrobial activity;
- Can maintain adequate silver ion concentrations for prolonged activity; and
- Do not contribute to antimicrobial resistance.
Nanosilver also exerts anti-inflammatory effects; however, mechanisms of this beneficial effect remain unknown.
“No studies specifically show a synergistic effect of topical honey and silver, but both can be used synchronistically,” Pantaleon says. “Furthermore, due to the multiple targets used by these products to kill microbes, the emergence of resistance by part of the microbes does not occur.”
Equine Wound Complications
A wide variety of complications can develop during wound management. Some of the more commonly observed short-term complications include:
- Local infection characterized by discharge, malodor, and fluid swelling (edema);
- Local infection characterized by discharge, malodor, and fluid swelling (edema);
- Cellulitis, an aggressive skin infection that can spread rapidly if left untreated;
- Local infection characterized by discharge, malodor, and fluid swelling (edema);
- Cellulitis, an aggressive skin infection that can spread rapidly if left untreated;
- Proud flesh/EGT;
- Local infection characterized by discharge, malodor, and fluid swelling (edema);
- Cellulitis, an aggressive skin infection that can spread rapidly if left untreated;
- Proud flesh/EGT;
- Delayed healing;
- Local infection characterized by discharge, malodor, and fluid swelling (edema);
- Cellulitis, an aggressive skin infection that can spread rapidly if left untreated;
- Proud flesh/EGT;
- Delayed healing;
- Laminitis, such as supporting-limb laminitis that can develop in the noninjured limb due to excess weight-bearing; and
- Local infection characterized by discharge, malodor, and fluid swelling (edema);
- Cellulitis, an aggressive skin infection that can spread rapidly if left untreated;
- Proud flesh/EGT;
- Delayed healing;
- Laminitis, such as supporting-limb laminitis that can develop in the noninjured limb due to excess weight-bearing; and
- Colic, due to a sudden lay-up, decreased exercise, and potentially an abrupt change in diet.

CREDIT: Shelley Paulson

CREDIT: Courtesy Dr. Kennon Keckler

CREDIT: Amy McLean

CREDIT: Courtesy Ryan Penno

CREDIT: Joanna Virgin

CREDIT: Anne M. Eberhardt/The Horse
Says Hendrickson, EGT is one of the most common complications that occurs following injury.
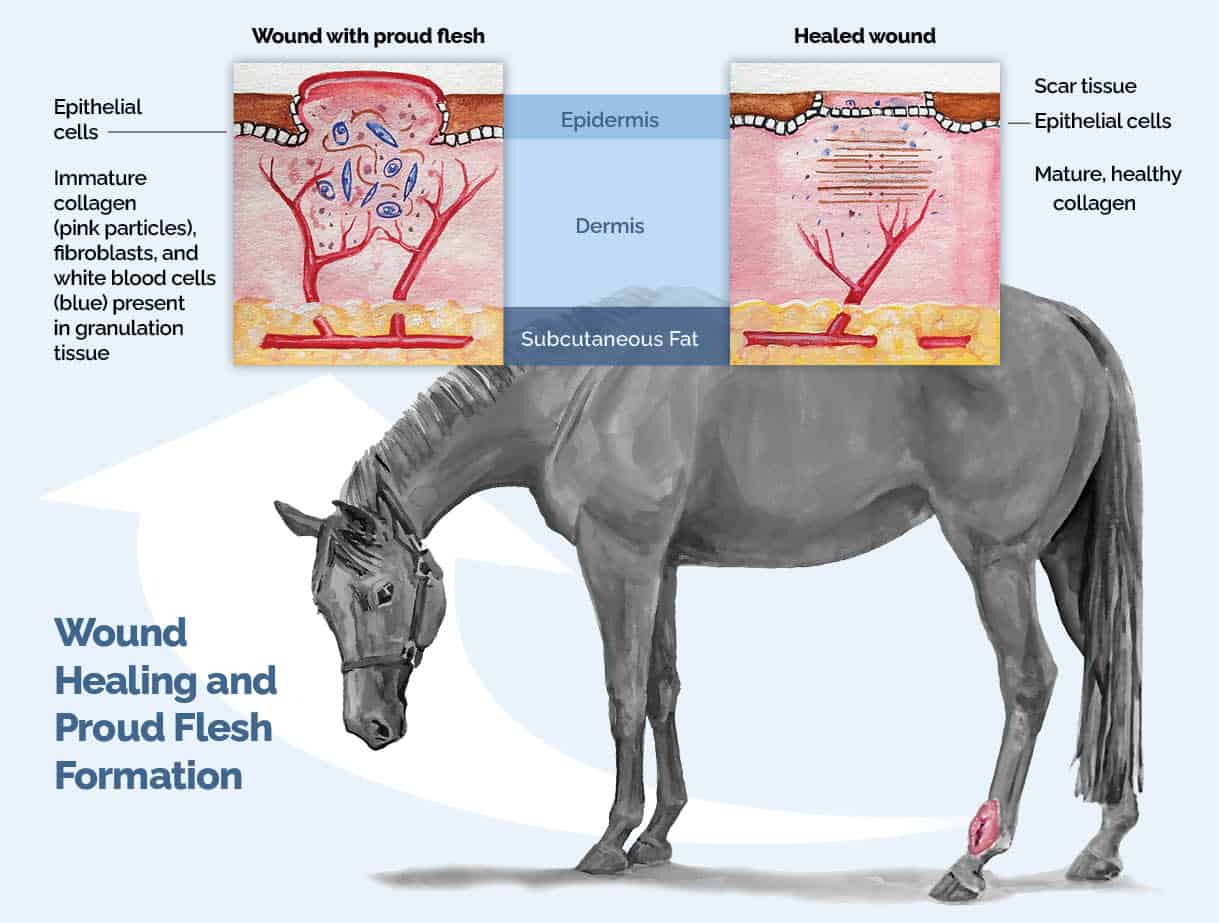
“Granulation tissue formation is actually a critical part of the wound healing process,” he says. “If there is a tissue defect, granulation tissue is required before the epithelium can migrate across the wound. When the granulation tissue is unhealthy, it forms an edematous bed of tissue that negatively impacts wound healing.”
“In other words, granulation tissue creates a scaffold on which healthy tissues can grow upon to heal the wound,” Pantaleon adds.
When the inflammatory phase of wound healing persists, excess granulation tissue forms. This tissue can be as minor as a slightly raised region at the wound site to an extensive, unaesthetic, bulbous growth of tissue that interferes with the horse’s function. Wounds on the distal (lower) limb or high-motion regions can essentially get stuck in the early phases of healing, promoting EGT. Owners should ask their veterinarians about the appearance of EGT.
“Proud flesh is generally due to infection and poor dressing techniques,” Hendrickson says. “Honey/silver or antibiotics actually decrease the likelihood of proud flesh, as long as the appropriate antibiotics are used and the appropriate dressing for moisture control is used. Dressings do not necessarily lead to more exuberant granulation tissue, just inappropriate dressings. Antiseptic use is often one of the worst things for causing exuberant granulation tissue.”
To prevent this serious and debilitating complication, Pantaleon recommends working with your veterinarian to address wounds properly and early in their course.
“Doing this will improve the chances for your horse to heal properly, return to its normal activity, and lower the cost of care,” Pantaleon says.
If proud flesh does develop, Hendrickson says the most important thing to do is have your veterinarian debride it.
Take-Home
Message
Skin wounds in horses occur frequently and can become significant financial and welfare concerns, especially if complications such as EGT develop. While antibiotics have been the mainstay for treating injuries in the past, the much-needed push for good antibiotic ambassadorship means more veterinarians and horse owners are managing wounds using antibiotic alternatives. Good debridement, avoiding antiseptics, and following your veterinarian’s instructions closely will maximize positive outcomes.
Tips for Good Antimicrobial Stewardship
According to Dr. Val Edwards-Jones, you can follow these tips to maximize antimicrobial drugs’ short- and long-term efficacy:
- Do not use antibiotics if they are not warranted;
- Complete the entire course of prescribed antibiotics to remove all the bacteria from the infected site;
- Do not stop antibiotics when a wound looks like it’s better; and
- Whenever possible, ask your veterinarian to take swabs to identify the offending pathogen (disease-causing organism) and prescribe correct treatment.
“In a perfect world, all wounds are cultured before using antibiotics and the most appropriate antibiotics are used,” says Dr. Dean Hendrickson. “Sometimes, though, the veterinarian needs to start antibiotics before receiving the culture/sensitivity results, but those antibiotics can later be modified if needed.”
Credits:

Stacey Oke
Stacey Oke, MS, DVM, is a practicing veterinarian and freelance medical writer and editor. She is interested in both large and small animals, as well as complementary and alternative medicine. Since 2005 she’s worked as a research consultant for nutritional supplement companies, assisted physicians and veterinarians in publishing research articles and textbooks, and written for a number of educational magazines and websites.
Editor-in-Chief: Stephanie L. Church
Digital Editor: Michelle Anderson
Editorial Team: Alexandra Beckstett
Art Director: Brian Turner
Digital Producer: Jennifer Whittle
Publisher: Marla Bickel






