by Katie Navarra and Michelle Anderson
Equine lameness associated with navicular syndrome can cause major frustration and expense for horse owners. When a horse isn’t sound, we fret over his long-term well-being and lament not being able to compete, train, or trail ride.
What is Navicular Syndrome?
So-called navicular or caudal heel syndrome is one cause of lameness that can appear in horses of any breed or discipline. It can be limited to one limb; however, it most commonly affects both front hooves, causing bilateral lameness. While veterinarians have documented it in the rear feet, these cases are very rare.
Horse people in general tend to lump all heel pain under the “navicular” umbrella, even though other issues might be to blame—hence the term “navicular syndrome,” says Dr. Tracy Turner.
It’s an overly simple name for a complex condition that we now know is most accurately described as podotrochlosis or podotrochleitis, because it can involve more of the podotrochlear apparatus than just the navicular bone, such as the navicular bursa or associated soft-tissue structures (e.g., the deep digital flexor tendon [DDFT] and collateral ligament of the distal interphalangeal joint [DIP or coffin joint]).
“It’s important to make this point because a more specific diagnosis allows for more specific treatment, and there are lots of different structures that may be injured in the pain syndrome,” he says.
Veterinarians believe navicular is caused by mechanical stress and strain due to the constant pressure between the navicular bone and DDFT, which leads to the degeneration of those and other structures that make up the podotrochlear apparatus. Poor foot conformation, such as a long toe and low heel, increases this stress and might potentiate development of the condition.
The result is lameness, which can become chronic. “It is characterized by shortness of stride, toe-landing, pain from the center third of the frog,” says Turner.
Early on these horses might present with a shortened stride right out of their stalls or while warming up, says Dr. Duncan Peters. “In more chronic cases, the horse that used to have a longer stride will become choppier and less fluid, because the horse is stabbing the toe to take the pressure off the back of the leg,” he says, describing the syndrome’s progression.
While any horse could develop podotrochlosis, research shows certain breeds, such as Thoroughbreds, Quarter Horses, and Warmbloods, are more at risk, and that it’s most commonly diagnosed in mature horses from 4 to 15 years old. Because of the relationship between hoof angles and the podotrochlear apparatus structures, hoof care, as well as conformation, can also contribute to the condition. Strain and sports-related injury from highly physical disciplines requiring hard turns, fast stops, lateral movement, and jumping, can also compound the problem, Peters says.
Initial signs can include the dressage horse that doesn’t want to lengthen or extend the trot, the hunter who starts knocking rails or stopping before jumps, or the horse that becomes unbalanced or nods its head when asked to trot a small circle, Peters says.
Better Imaging Has Led to Better Understanding of Navicular Syndrome in Horses
There’s no cure for this condition; rather, it’s about managing affected horses’ comfort. In recent years the prognosis for podotrochlosis has improved significantly due to the increased use of magnetic resonance imaging (MRI) and better communication between veterinarians and farriers to determine what is best for the horse, says Dr. Craig S. Lesser, an associate veterinarian in Rood & Riddle Equine Hospital’s podiatry department, in Lexington, Kentucky.
New therapies have also emerged that could be invaluable for managing these horses and returning them to work.
“The term navicular terrifies people,” says Lesser. “I try to avoid using navicular in exchange for what the true culprit of injury is. However, it doesn’t mean the end of a horse’s athletic performance.”
In this article Lesser, Peters, and Turner will explain what has remained the same and what’s changing when it comes to diagnosing and treating these injuries.
Tracy Turner
DVM, MS, Dipl. ACVS, ACVMR

Dr. Tracy A. Turner operates Turner Equine Sports Medicine and Surgery, in Stillwater, Minnesota, which focuses on lameness, sports medicine, and surgery. He has served as an Olympic, World Equestrian, and Pan American games veterinarian.
Duncan Peters
DVM, Dipl. AVSMR

Dr. Duncan Peters is co-owner and co-founder of East-West Equine Sports Medicine, which offers services in Kentucky and California. He is a multi-discipline licensed Federation Equestrian Internationale (FEI) veterinary delegate.
Craig Lesser
DVM, CF

Dr. Craig Lesser is an associate veterinarian at Rood & Riddle Equine Hospital, in Lexington, Kentucky. Lesser has an interest in podiatry, lameness, and imaging. He also enjoys teaching, volunteering, doing research, and continuing to further his education.
Diagnosis
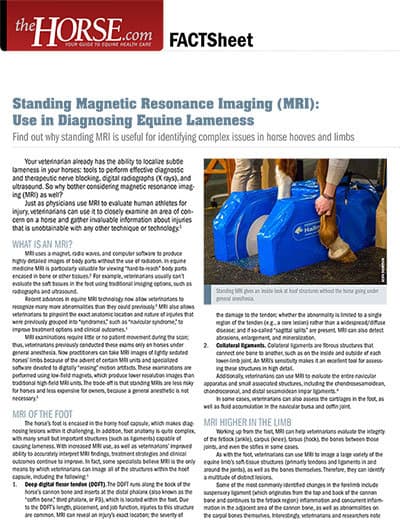
Technological advancements have given us a clearer picture of the navicular-related changes taking place within the horse’s hoof. Magnetic resonance imaging has become the gold standard for determining which structures are involved and the extent of damage, Lesser says. This imaging tool is the first that truly allows us to thoroughly view the components within the horse’s hoof and the changes occurring in them. One of the lessons MRI has already taught us is that there are many injuries and combinations of injuries that result in “navicular” lameness, says Turner.
Radiographs (X rays) are still important for examining the hoof’s bony structures and changes that are occurring. However, researchers have found in sound horses some of the same radiographic changes lame horses have.
“Depending on the type of horse, their age, and workload, some radiographic changes may be within normal limits and not causing lameness,” Lesser says.
In some cases a bursogram is also helpful. In this procedure, says Turner, the veterinarian injects a dye into the navicular bursa (the cushioning fluid-filled sac between the navicular bone and the deep digital flexor tendon that runs from the back of the knee down around the navicular bone) to illuminate it, the cartilage, and the bursa edge of the deep digital flexor tendon on radiographs.
“This test can show anything from completely normal to adhesions of the tendon to the bone and even tendon injuries if the injury communicates with (affects or transfers to) the bursa,” he says.
Turner says a bursogram can be especially helpful when working up mounts used for lower-impact sports, such as trail riding. These horses can be difficult to diagnose because they perform long, slow mileage and might only be used sporadically, he says. Therefore, the rider doesn’t notice any change until out on the trail.
Peters adds that, in some cases, clinicians can also use ultrasound to image the soft tissue structures of the lower limb, such as the deep digital flexor tendon or the impar ligament, which could be involved with the lameness. “It’s not just about the navicular bone,” he reemphasizes.
A Hands-On Lameness Exam
Unfortunately, X rays, again, are limited to bony structures, and ultrasound—which veterinarians use to look at soft tissue structures—can’t provide a complete representation of what’s within the hoof. Additionally, says Peters, MRI isn’t a viable first diagnostic option for all horse owners due to cost and access to clinics that offer MRI services.
“People rely too much on the imaging and less on the examination, which (in my opinion) is more important,” Turner says. “Also, as we are able to identify pathology (disease or damage), we are not able to necessarily determine how significant it is.”
For that reason, all three veterinarians start every evaluation with a thorough hands-on lameness exam that includes a visual analysis of the hoof and its abnormalities, along with palpation and flexion tests.
During a lameness exam, Peters likes to evaluate the horse on the longe line or under saddle to see how it moves. He also prefers watching the horse on both hard (asphalt) and soft (arena sand) surfaces. Comparing how the horse moves on both surfaces “allows us to appreciate the changes between the two,” Peters says. For example, the horse might have an exaggerated head bob and longer flight time on the affected leg due to the added concussion from trotting on hard ground.
“Part of the assessment is looking at the biomechanics of the hoof, how the horse stands, shapes of walls, shape of the foot, and shape of the frog,” Turner says.
Hoof testers are also an important tool early in the diagnostic process, says Lesser.
“Hoof testers are one of the most valuable tools in localizing injury to the hoof,” says Lesser. “Many—but not all—horses will be sensitive to hoof testers over the frog and heels if they have navicular region injury.”
Distal (lower) limb flexion tests are also part of this exam. Turner says 90% of all chronic foot lamenesses he sees flex positive. With a bilateral forelimb lameness, he injects local anesthetic over the palmar digital nerves in the low pastern area of one limb, called a palmar digital nerve block.
“You will see how truly lame the horse is because now you see lameness in only one leg, the unblocked leg,” he says. “The owner/rider is often shocked at how sore the horse really was.”
Turner also uses a wedge test, in which he places a 1-inch-thick block under the frog, the toe, and the inner and outer hoof walls for about 60 seconds, then trots the horse off to evaluate lameness. He measures the horse’s response to each elevation change and rates the degree of lameness on a scale of 1 to 5.
“These tests are important because they give clues as to where and how the horse perceives pain,” Turner says.
Because podotrochlosis can encompass a wide range of painful changes in the hoof, the lameness exam combined with diagnostic imaging are critical to determining the source of pain and developing a treatment plan for the horse.

Treatment
Podotrochlosis often requires a multipronged treatment approach that might include rest, drug treatment, shock wave therapy, and hoof care that improves hoof angles, among others. “There are a lot of options,” Peters says. His goal is to create a treatment and management plan that works for the individual horse.
For acute pain, a veterinarian might prescribe a non-steroidal anti-inflammatory drug (NSAID) such as bute or firocoxib to help make the horse more comfortable and break the conditions initial pain cycle, Peters says.

Bisphosphonates are another drug treatment option for specific navicular syndrome cases. These medications essentially reduce bone remodeling and the pain associated with it and were originally developed to treat osteoporosis in humans. The U.S. Food and Drug Administration (FDA) has approved two bisphosphonate drugs specifically for treating navicular syndrome.
According to The Horse’s Fact Sheet “Bisphosphonate Use in Horses”:
“In healthy animals, including horses, bone turns over continually.
Cells called osteoclasts play a key role in breaking down old bone
while another type of cell—osteoblasts—creates new bone. This natural process ensures bones remain strong and healthy and allows them
to adapt to changes in exercise level or musculoskeletal system stress.
Bisphosphonates bind to osteoclasts to block excess bone resorption. “
Because bisphosphonates target bone rather than soft tissue, proper diagnosis to pinpoint the cause of podotrochlosis (i.e., soft tissue injury vs. bone disease or injury) is important for determining if bisphosphonates are right for a specific case, Peter says. “They’re one of our better treatment options for horses with bony problems or bone inflammation,”he said.
Lesser notes that bisphosphonates can cause colic and negatively affect the kidneys. Additionally, he notes, they should not be administered with NSAIDS. “Bisphosphonates and NSAIDS are both drugs that are excreted by the kidneys,” he explains. “If these drugs (together) put too much stress on the kidneys, the concern is that they could be nephrotoxic.”
Another approach (gaining popularity in the early 2000s) is extracorporeal shock wave therapy. Shock wave, like bisphosphonates, can be a useful part of the horse’s management plan but is not and should not be the main therapy, says Turner.
“For me, shock wave helps break the pain cycle and gets the horse to move in a more normal fashion,” he says. “It can be helpful in the overall management, but (it’s not) going to cure the problem.”
Shock wave therapy emits high-intensity sound waves that can have a pain-relieving effect and might reduce healing time for ligamentous and tendinous injuries. To be effective the treatment must focus specifically on the painful or injured area.
Lesser says shock wave therapy is useful when MRI shows signs of injury to structures such as the impar ligament, which attaches the navicular bone to the coffin bone and the suspensory ligament.
Trimming and Shoeing Are Priority
While new medical treatments offer promising outcomes, Lesser and Turner agree that trimming and shoeing are the first steps in managing horses with podotrochlosis.
“I tend to start with shoeing changes to see how much improvement we can achieve with shoeing alone,” Lesser says.
Radiographs can guide trimming and shoeing decisions. They help the veterinarian and farrier determine exactly how much foot they can manipulate, Lesser says.
One of the first shoes he reaches for is a wedged shoe with a welded heel plate. He says this shoe’s wedge reduces the tension on the deep digital flexor tendon that uses the navicular bone as a fulcrum. The heel plate helps prevent shock from transmitting directly through the frog and up to the navicular region.
“Many of these horses are also placed in a (slight) full rocker to decrease leverage at breakover (the point at which the heel lifts off the ground during movement) and decrease concussion at landing,” Lesser says.
Turner says he considers the horse’s conformation and foot shape when selecting shoes. There is not a hard-and-fast formula farriers can refer to, such as simply applying a bar shoe or raising the heels. They must base the trimming and shoeing protocol on the hoof’s biomechanical needs and what changes can be made to relieve pain and allow the hoof to function at its best. Shoe selection for horses with podotrochlosis also depends on discipline and disease severity, he adds.
Additional Pain Management
After trimming and shoeing, if additional pain management is necessary, Turner says veterinarians can inject two synovial cavities inside the hoof capsule with anti-inflammatory drugs.
He says he injects the coffin joint if the distal limb flexion was the most positive manipulative test or the navicular bursa if the frog wedge was positive. Other veterinarians prefer to have MRI dictate injections.
Once the horse starts feeling good, Turner emphasizes the importance of putting him back into work.
“Work and stress will help restore the hoof biomechanics; standing in a stall won’t help,” Turner says. “The horse must be reassessed after to make sure that (restoration has happened) and that they are not painful.”
Podotrochlosis is complicated to manage. There is no one-size-fits-all treatment, and it requires continual follow-up and adjustments as needed.
“Because this is a complex condition, we must quit thinking of a single treatment and we must think in terms of what we are treating,” Turner says.
Case 1: Brandy: 12-year-old Oldenburg gelding used for eventing
When Brandy, who’s usually eager to work, started refusing fences in jump schools and not going forward in the dressage ring, his owner knew something was wrong.
She called Turner, who ran through the set of diagnostic procedures he performs on any horse he suspects of having navicular-related problems: observation of the hoof, lower limb flexion tests, wedge tests, and nerve blocking. On this horse the flexion was the most positive indicator of a navicular issue. Radiographs looked normal for a horse of Brandy’s age, breed, and use.
Initially, Turner made minor adjustments to the gelding’s shoeing and injected his coffin joints. But Brandy did not respond as expected. While he improved some, he didn’t stay sound. The next step was to perform an MRI.
The MRI showed fluid accumulation (edema) in the navicular bone, along with other minor changes. The most significant “change,” however, was the edema.
“Edema like this is a sign of bone remodeling within the navicular bone,” he says. “We added bisphosphonate therapy to our treatment protocol, and within 30 days the horse had returned successfully to eventing.”
He examines Brandy, reassesses the horse’s therapeutic needs, and administers bisphosphonates about every six months. With this approach he and the owner are managing the gelding’s needs at this time.
Case 2: Cappy: 7-year-old Quarter Horse mare used for trail riding
Trail horses like Cappy usually do long, slow mileage and might only be ridden sporadically. This means the rider might not notice subtle soundness issues until out on the trail.
“Cappy’s owner called me because the mare was reluctant to go down hills,” says Turner.
In addition to his normal podotrochlosis diagnostic process, Turner performed a bursogram and took radiographs.
This was helpful because in Cappy’s case, the changes seen on radiographs were within normal expectations, but the bursogram showed significant fraying of the deep digital flexor tendon where it passes the navicular bursa.
Shoeing changes were critical to keeping Cappy sound. These included a wide web shoe with a rockered toe and pour-in sole packing to distribute weight over more of the foot. Turner also injected her navicular bursa.
The mare responded well to these adjustments, although not all do, says Turner. She went back to work as a useful trail horse. Turner reassesses her soundness periodically.
Case 3: Sonny: 16-year-old senior pleasure horse
Senior horses with navicular issues can be challenging to diagnose. If the lameness is in both front feet, for instance, the owner might not notice it right away, chalking any stiff movement up to age. Also, it’s common that these horses aren’t being ridden regularly, which is when most owners pick up on irregularities. So, the onset is gradual and difficult to discern until the horse is really lame.
When Turner first examined Sonny, he noticed the gelding was short-strided in front and choppy when trotting. As the owner rode in circles, Sonny became increasingly more lame as the circles became smaller.
“It was really noticeable when he trotted on a hard surface; that’s when you could see the shortened stride,” Turner says.
The horse was equally short-strided on both forelimbs and appeared particularly sore on the inside leg, regardless of direction. Turner’s exam included a flexion test and a wedge test. The most significant finding came during the frog wedge test, which exacerbated the lameness markedly on each foot. When Turner blocked Sonny’s right front leg, the horse was a Grade 2 of 5 left forelimb lame.
“The owner was shocked at how sore the horse really was,” he says.
Shoeing changes improved Sonny’s weight-bearing on the caudal (rear) half of the hoof and made movement easier. In addition, Turner injected the navicular bursa with a mixture of corticosteroids. Sonny resumed light work and is scheduled for a reassessment to continue managing the condition.
Prevention
Podotrochlosis is a chronic lameness that creates permanent changes. Because it has no cure, prevention is ideal. Maintaining a regular trimming and/or shoeing schedule with a skilled farrier keeps the horse’s hoof in the correct proportions.
“The best way to prevent it is to have a farrier that can put the best foot on that horse,” Turner says.
Early detection is as important as prevention, he adds. If you notice anything—a change in the horse’s gait or attitude toward work—don’t ignore it. Have your veterinarian assess the horse.
 Katie Navarra
Katie Navarra
Katie Navarra has worked as a freelance writer since 2001. A lifelong horse lover, she owns and enjoys competing a dun Quarter Horse mare.
 Michelle Anderson
Michelle Anderson
Michelle Anderson is the former digital managing editor at The Horse. A lifelong horse owner, Anderson competes in dressage and enjoys trail riding. She’s a Washington State University graduate and holds a bachelor’s degree in communications with a minor in business administration and extensive coursework in animal sciences. She has worked in equine publishing since 1998. She currently lives with her husband on a small horse property in Central Oregon.
Editor-in-Chief: Stephanie L. Church
Digital Managing Editor: Michelle Anderson
Editorial Team: Alexandra Beckstett, Erica Larson
Art Director: Brian Turner
Digital Producer: Jennifer Whittle
Illustrator: Claudia Summers
Publisher: Marla Bickel





