Risk Factors for Colic Surgery Incision Failure Studied
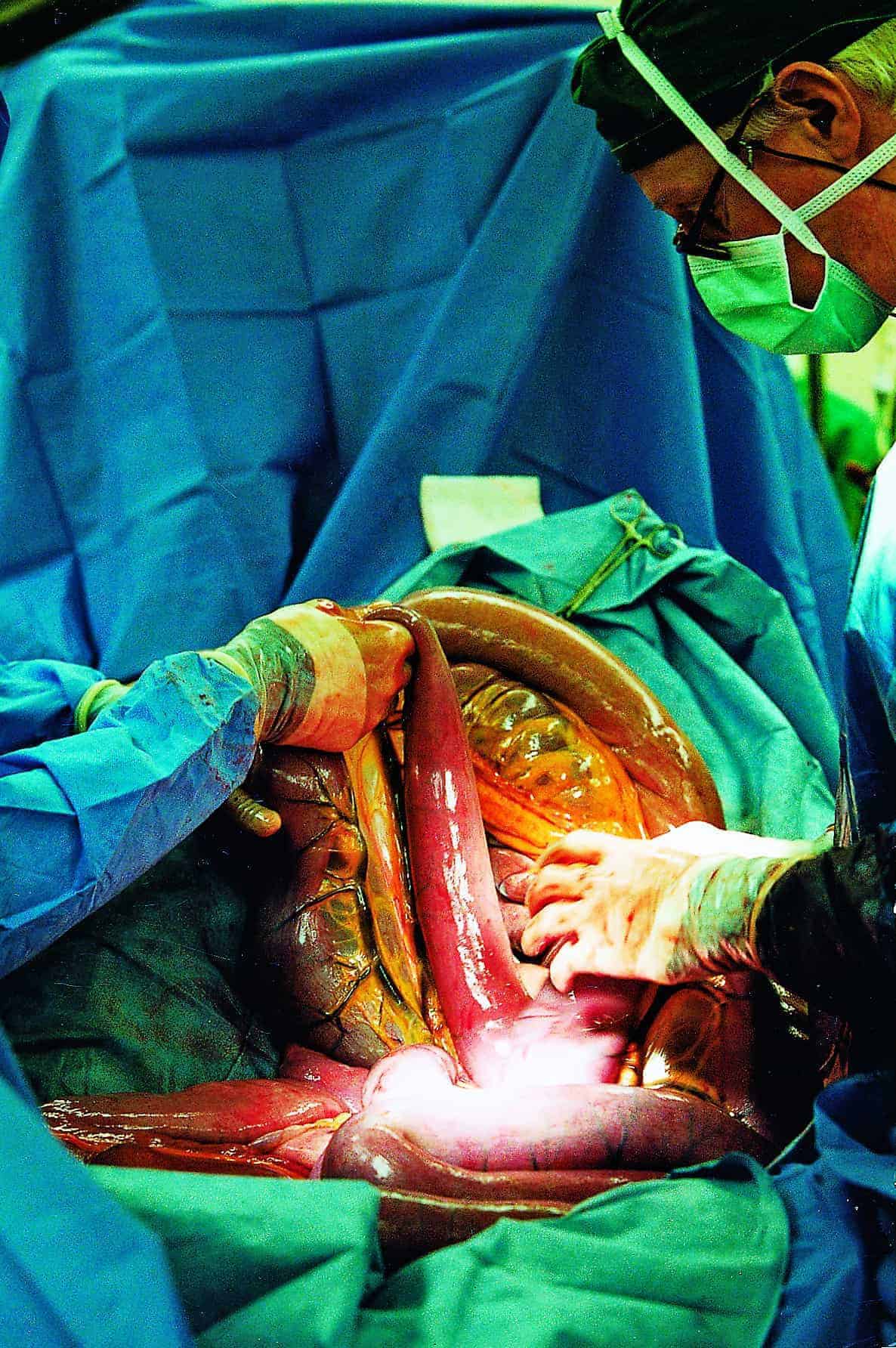
In the best-case scenario, the surgeon can clean up and resuture the incision without additional complications. In the worst-case scenario, too much damage occurs and the horse must be euthanized.
While veterinarians monitor all patients for signs of incision failure, it hasn’t been clear which, if any, cases are at greater risk for complications or what factors influence survival following incision failure. So, Alison Gardner, DVM, MS, Dipl. ACVS-LA, an assistant professor at The Ohio State University (OSU) College of Veterinary Medicine Department of Veterinary Clinical Sciences, in Columbus, recently completed a study on the topic. She shared the results at the 2017 International Equine Colic Research Symposium, held July 18-20, in Lexington, Kentucky.
Gardner and colleague Margaret Mudge, VMD, Dipl. ACVS, ACVECC, a clinical associate professor at the OSU College of Veterinary Medicine, reviewed 10 years of medical records to identify risk factors for acute ventral midline dehiscence and evaluate survival after wire placement to re-close the incision
Create a free account with TheHorse.com to view this content.
TheHorse.com is home to thousands of free articles about horse health care. In order to access some of our exclusive free content, you must be signed into TheHorse.com.
Start your free account today!
Already have an account?
and continue reading.

Written by:
Erica Larson
Related Articles
Stay on top of the most recent Horse Health news with











